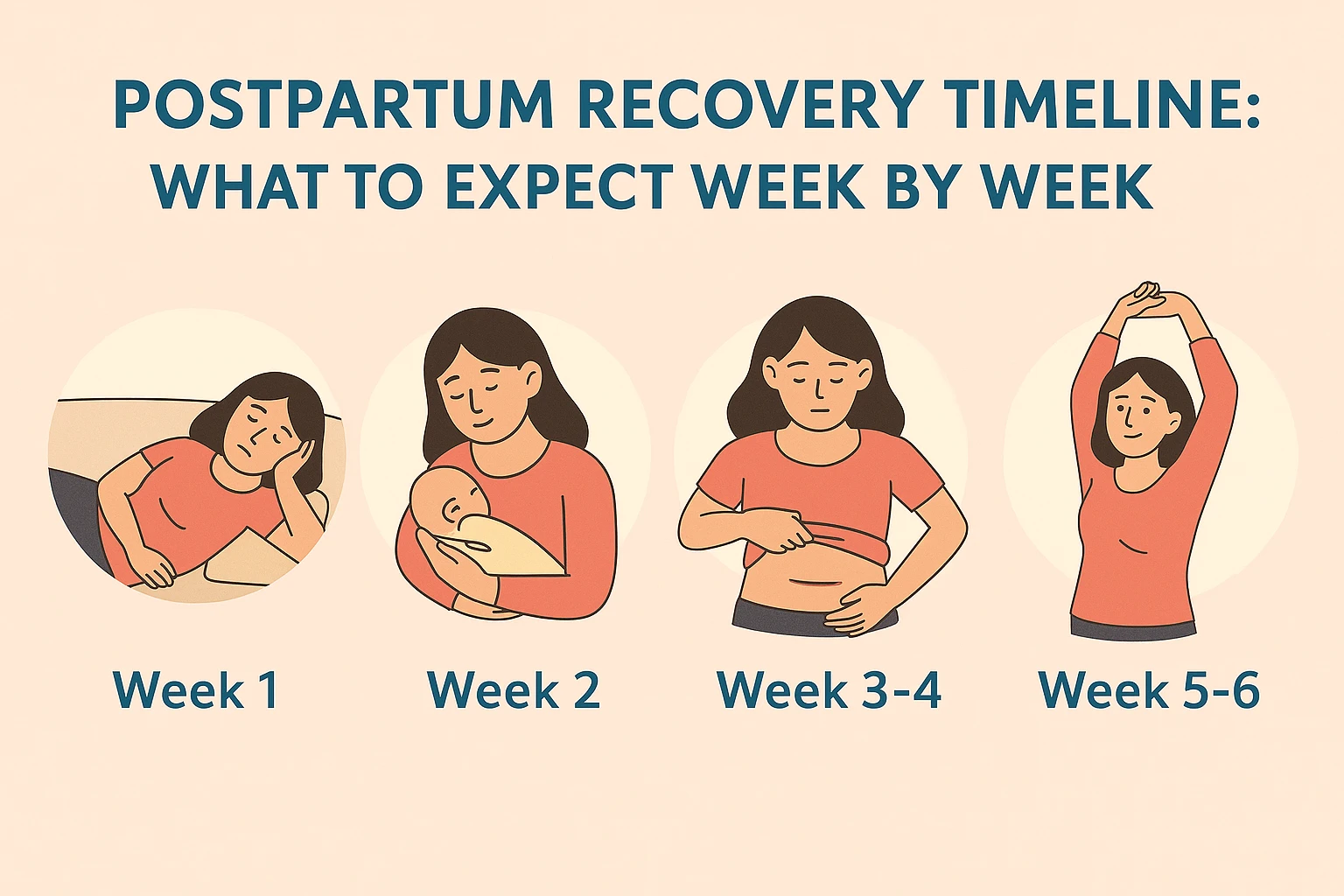
Postpartum Recovery Timeline: What to Expect Week by Week (The Fourth Trimester Guide)
The fourth trimester is about healing. This detailed guide breaks down the postpartum recovery timeline, explaining physical healing, hormonal shifts, and emotional milestones from Week 1 to 6 months.
Try Related Tools
Use our medically reviewed calculators to get accurate insights.
You have just completed the marathon of pregnancy and labor. While the focus has rightfully shifted to your newborn, your body is embarking on its next great journey: The Fourth Trimester—the 12-week period immediately following birth.
This time is often characterized by intense physical healing, dramatic hormonal shifts, and overwhelming emotional changes. Society often focuses on the baby's milestones during this period, but your healing deserves equal attention.
There is no single "normal" timeline for postpartum recovery, as every birth (vaginal, C-section, or multiples) and every body is unique. However, understanding the general recovery arc can help you manage your expectations and recognize when something needs medical attention.
This guide provides a comprehensive week-by-week timeline of what to expect as your body heals, emotionally and physically.
Table of Contents
- CRITICAL: When to Call Your Doctor IMMEDIATELY
- Phase I: The Immediate Fourth Trimester (Weeks 1-6)
- Phase II: The Recovery Phase (Weeks 7-12)
- Phase III: Long-Term Healing (Months 3-6+)
- Your Plan for a Healthy Recovery
CRITICAL: When to Call Your Doctor IMMEDIATELY
Postpartum complications can be serious. Do not wait to seek medical attention if you experience any of these red flags:
- Heavy Vaginal Bleeding (Hemorrhage): Soaking through more than one large sanitary pad per hour for two hours or more, or passing clots larger than a golf ball.
- Severe, Persistent Headache: A headache that doesn't go away with medication, or one accompanied by vision changes or light sensitivity (possible sign of preeclampsia).
- High Fever: A temperature of 100.4°F (38°C) or higher.
- Severe Pain: Unbearable pain in the abdomen, chest, or pelvis that is not relieved by prescribed medication.
- Painful Swelling or Redness in Legs: Pain, tenderness, or swelling in one leg (possible sign of a deep vein thrombosis/blood clot).
- Thoughts of Harming Yourself or Your Baby: Call emergency services or a dedicated helpline immediately.
Phase I: The Immediate Fourth Trimester (Weeks 1-6)
This phase is about triage, rest, and bonding. The primary goal is healing the physical trauma of birth and managing the rapid crash of pregnancy hormones.
Week 1: The Crash and the Cleanse
- Physical Healing: Your uterus, which was the size of a watermelon, begins the rapid process of shrinking back to its pre-pregnancy size. This causes afterpains (contractions similar to mild period cramps).
- Lochia (Bleeding): Vaginal bleeding (lochia) is heavy, bright red, and contains clots. This is the shedding of the uterine lining and will continue for several weeks.
- Wound Care: For a vaginal birth, stitches from tearing or an episiotomy are often the most painful. For a C-section, the incision site is swollen, tender, and requires careful cleaning.
- Hormonal/Emotional: Progesterone and estrogen levels drop dramatically, leading to the "baby blues"—mood swings, irritability, and crying spells. This usually peaks around Day 3-5.
Week 2: Finding a Rhythm
- Physical Healing: Pain is usually manageable with over-the-counter medication. Lochia starts to lighten in color (pinkish-brown) and volume. C-section stitches may be healing well, though the area remains tender and numb.
- Emotional Focus: You are mastering the basics of newborn care and navigating severe sleep deprivation. Your mood should stabilize after the baby blues fade.
- Activity: Focus on pelvic floor exercises (Kegels) and gentle walking around the house. Still no lifting anything heavier than your baby.
Weeks 3-4: The Turnaround Point
- Physical Healing: Lochia continues to lighten and may now be yellowish or white. Most stitches (vaginal or C-section) have dissolved internally. Swelling in the legs and feet should subside as your body sheds excess pregnancy fluid.
- Emotional Focus: Many partners return to work, and the reality of solo newborn care sets in. Fatigue is immense.
- Activity: You may feel ready for gentle walks outside. Crucial: Avoid high-impact exercise (running, jumping) and core work (crunches) to protect your pelvic floor and check for Diastasis Recti.
Weeks 5-6: Medical Clearance
- Physical Healing: Lochia should be very light or finished. The 6-week postpartum check-up is scheduled. This is when your doctor assesses your healing, examines your incision (C-section), checks your cervix, and clears you for exercise and sexual activity.
- Emotional Focus: You should be feeling more like yourself, but the demands of a newborn can lead to isolation and anxiety. Screen for persistent depression or anxiety.
- Activity: Once cleared by your doctor, you can gradually reintroduce gentle, intentional exercise. Do not jump right into your pre-pregnancy routine.
Phase II: The Recovery Phase (Weeks 7-12)
This phase begins after medical clearance and focuses on gradually rebuilding strength and integrating physical activity back into your life.
Weeks 7-8: Core Reconnection
- Physical Healing: You are physically cleared, but your body is still structurally weak. Focus shifts to the core.
- Diastasis Recti (DR): The separation of the abdominal muscles (rectus abdominis) is common. Start checking your core for this separation and work only on deep core exercises (like pelvic tilts and transverse abdominis breathing). Avoid anything that strains the abs.
- Wellness Focus: Establishing consistent sleep hygiene and asking for help are key to preventing burnout.
Weeks 9-12: Building Endurance
- Physical Healing: You can start working on endurance. Low-impact cardio is safe: using an elliptical, stationary cycling, or power walking. Continue avoiding running or jumping until you have full core stability and no pelvic pain whatsoever.
- Emotional Focus: This is a common time for Postpartum Depression (PPD) or Postpartum Anxiety (PPA) to surface. Fatigue, guilt, or feeling disconnected from your baby are not normal—they are symptoms that require professional support.
- Activity: Slowly increase the duration of your workouts, but keep the intensity moderate.
Phase III: Long-Term Healing (Months 3-6+)
Recovery doesn't end at 12 weeks. Full recovery often takes 6 months to a year, especially for core and pelvic floor strength.
Months 3-4: Returning to Strength
- Physical Healing: If your core is stable and you have no vaginal heaviness or pain, you may be cleared for light running. If you had a C-section, the internal incision is still healing, so listen to your body and watch for any pain around the scar.
- Fitness Goal: Prioritize strength over cardio. Focus on compound movements (squats, lunges, deadlifts) with low weight, as these recruit the entire core and help stabilize your joints.
Months 5-6: Full Integration
- Physical Healing: Your hormones are stabilizing. Your hair loss (which peaks around 3-4 months) may begin to slow down.
- Wellness Focus: Re-evaluate your relationship with your body. Focus on self-compassion, not "bouncing back." Full healing involves accepting the physical changes as part of the journey.
Beyond 6 Months
- The Reality: The American Physical Therapy Association states it takes 6 months to 1 year for the pelvic floor, core, and ligaments to fully regain their non-pregnant strength. Be patient with your body.
- Final Steps: If you still experience pain, urinary leakage, or significant abdominal separation beyond 6 months, consult a Pelvic Floor Physical Therapist (PT). This specialized help can be life-changing and is often the final step to full recovery.
Your Plan for a Healthy Recovery
The best way to navigate the often-turbulent Fourth Trimester is by having a clear plan and knowing what you need each day.
The first step is establishing a checklist of essential needs—from pain management to feeding schedules and mental health checks—to ensure you are prioritizing your healing along with your baby's care.
Get Your Healing on Track
Don't let your recovery be an afterthought. Use our simple, comprehensive Postpartum Recovery Checklist to track your progress, identify essential tasks, and ensure you're addressing every aspect of your healing journey.
Medical Disclaimer
The information in this article is for informational and educational purposes only and is based on general medical guidelines. It is not a substitute for professional medical advice, diagnosis, or treatment. Postpartum recovery is unique. Always follow the specific instructions of your physician, midwife, or qualified healthcare provider regarding your recovery timeline and exercise clearance.
About the Author
Abhilasha Mishra is a health and wellness writer specializing in women's health, fertility, and pregnancy. With a passion for empowering individuals through evidence-based information, she writes to make complex health topics accessible and actionable.