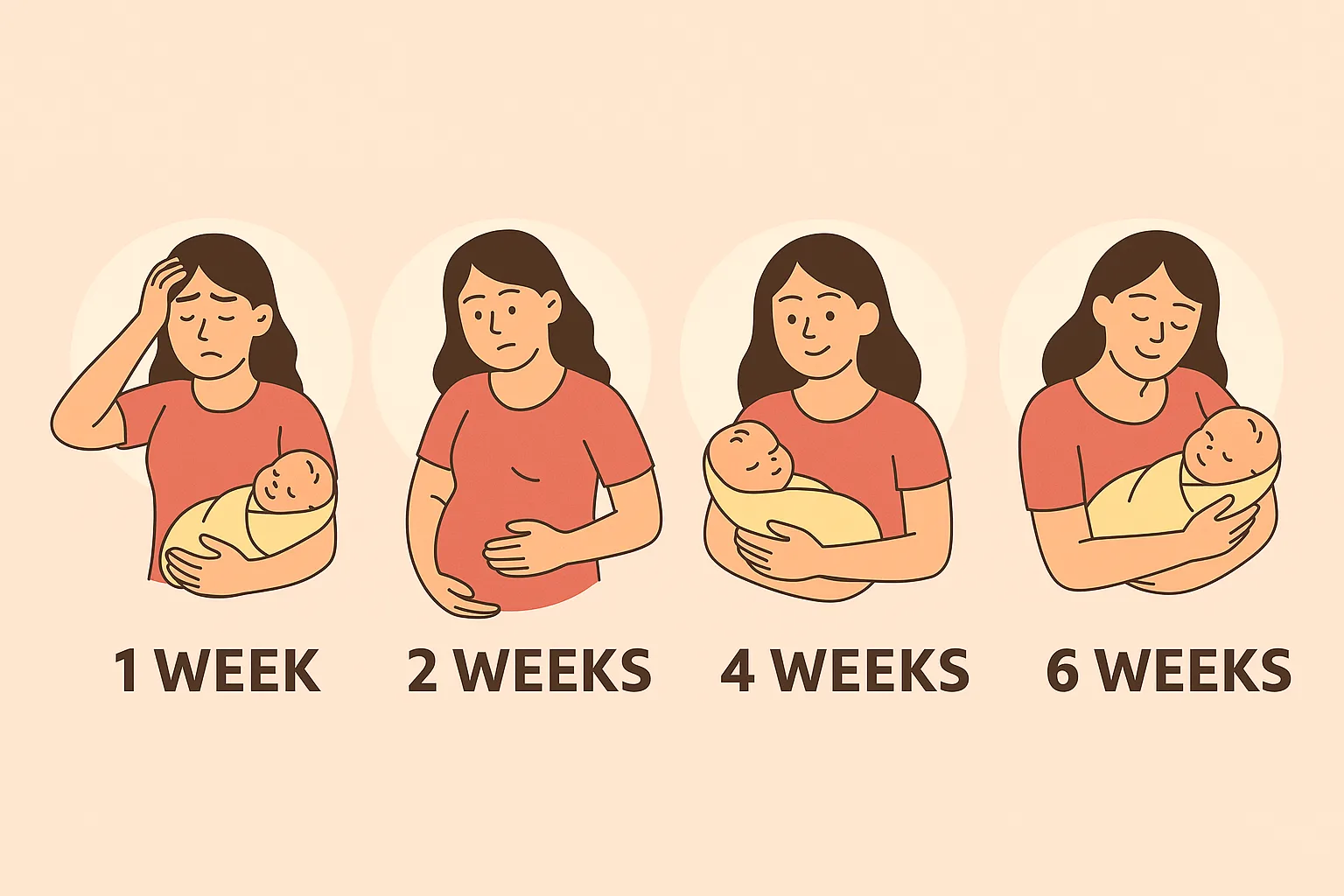
Your First 6 Weeks After Birth: A Realistic Healing Timeline
The 'fourth trimester' is a period of intense physical and emotional change. We break down exactly what happens to your body week by week, from lochia and hormone crashes to the six-week checkup.
Try Related Tools
Use our medically reviewed calculators to get accurate insights.
You have spent nine months growing a life and hours (or days) laboring to bring it into the world. Congratulations, you are a mother! But as the adrenaline of birth fades and you settle in with your newborn, you might find yourself surprised by the physical aftermath.
Society often glosses over the reality of the "fourth trimester." We see images of celebrities "bouncing back" in weeks, which sets an impossible and unhealthy standard. The truth is, your body has just undergone a major medical event. Whether you had a vaginal delivery or a C-section, you have a wound the size of a dinner plate inside your uterus (where the placenta detached), your organs are shifting back into place, and your hormones are taking a skydive.
Healing is not a linear process, and it certainly does not happen overnight. It is messy, emotional, and sometimes painful. But knowing what to expect can turn fear into empowerment.
Let us walk through a realistic, medically grounded timeline of your first six weeks, so you can give yourself the grace and care you deserve.
Table of Contents
- Week 1: The Adrenaline Crash and Physical Triage
- Week 2: The Hormone Drop and "Baby Blues"
- Week 3: The Turning Point
- Week 4: The "Normal-ish" Phase
- Week 5: The Mental Game
- Week 6: The Check-Up Milestone
- Frequently Asked Questions (FAQ)
- A Note on Patience
Week 1: The Adrenaline Crash and Physical Triage
The first week is often a blur of joy, exhaustion, and physical soreness. You are running on adrenaline and love, but your body is in triage mode.
What is Happening Physically:
- Lochia (Bleeding): You will experience heavy vaginal bleeding, known as lochia. In these first few days, it will be bright red and heavy, perhaps with some small clots. This is your body shedding the uterine lining.
- Afterpains: You might feel cramping as your uterus shrinks back down (involution). These cramps can be surprisingly intense, especially while breastfeeding, as oxytocin triggers contractions.
- Perineal or Incision Pain: If you had a vaginal birth, your perineum is likely swollen and sore, especially if you had tearing or an episiotomy. If you had a C-section, your incision site is fresh surgery. Movement will be difficult. For specific advice on managing surgical recovery, read our C-Section Recovery Tips Guide.
What You Need to Do: Rest is not a luxury; it is a medical necessity. Stay in bed or on the couch as much as possible. Focus on hydration and pain management. Do not try to be a host to visitors.
Tip: Use ice packs for perineal swelling and keep a peri-bottle handy for bathroom trips. If you are struggling with incision pain, check out our blog on How to Recover Faster After C-Section for safe movement strategies.
Week 2: The Hormone Drop and "Baby Blues"
By the second week, the initial adrenaline has worn off, and the reality of sleep deprivation sets in. This is also when the biggest hormonal shift occurs.
The Emotional Rollercoaster: Estrogen and progesterone levels drop dramatically after birth. This chemical crash leads to the "Baby Blues" in about 80% of mothers. You might feel weepy, irritable, or anxious over small things. This is normal and usually temporary. However, it is crucial to know the difference between blues and something more serious. Read our article on Postpartum Mood vs. Depression to understand the warning signs.
Physical Changes:
- Night Sweats: You might wake up soaked. Your body is shedding the extra fluid it held during pregnancy.
- Breast Changes: Your milk usually comes in around day 3-5, leading to engorgement. Your breasts may feel rock hard, hot, and painful. Proper latching is key here. If you are in pain, consult our Breast Care and Pain Relief Guide for immediate soothing techniques.
Week 3: The Turning Point
For many women, week three feels like a turning point. You are starting to find a rhythm with the baby, and the acute physical pain is subsiding.
Healing Progress:
- Lochia Changes: The bleeding should be slowing down and changing color from bright red to pinkish-brown.
- Stitches: If you had stitches, they may start to itch as they heal. This is a good sign!
- Activity: You might feel ready for a short walk around the block. Listen to your body. If bleeding increases after activity, you did too much.
Nutrition Focus: Now that your appetite might be returning, fueling your recovery is vital. Your body needs protein and iron to repair tissues and replenish blood loss. Focusing on nutrient-dense foods can speed up healing. See our Postpartum Nutrition Guide for meal ideas that support tissue repair and milk supply.
Week 4: The "Normal-ish" Phase
You are one month postpartum! You might look in the mirror and start to recognize yourself again, though your body has changed.
Physical State:
- Uterus Size: Your uterus is almost back to its pre-pregnancy size.
- Energy: You might have bursts of energy, but fatigue is still a major factor due to broken sleep.
- Weight: You may have lost a significant amount of "water weight," but do not stress about the rest. It took nine months to gain; it won't disappear in four weeks. For a healthy perspective, revisit our blog on Managing Weight Gain in Pregnancy to understand the biological necessity of those stores.
If you are curious about tracking your progress healthily, you can use our Postpartum Weight Tracker, but remember: functionality matters more than the number on the scale.
Week 5: The Mental Game
Physically, you are much stronger. Ideally, the bleeding has stopped or is very light (yellowish/white). Mentally, however, the isolation can set in. Partners often return to work around this time, leaving you solo parenting.
Self-Care is Crucial: This is a high-risk time for burnout. Ensure you are still prioritizing your nutrition and rest. Connect with other moms or friends. It is okay to ask for help.
Pelvic Floor Awareness: You might notice your core feels weak. This is the time to start gentle pelvic floor engagement (like deep breathing), but avoid heavy lifting or high-impact exercise until you are cleared.
Week 6: The Check-Up Milestone
This week marks the traditional end of the "recovery" period, but we know healing continues long after. You will likely have your postpartum check-up with your provider.
What Happens at the Visit:
- Physical Exam: Your doctor will check your incision (if C-section) or perineal healing. They will feel your uterus and check for diastasis recti (abdominal separation).
- Mental Health Screen: Be honest about how you are feeling.
- Clearance: You typically get the "green light" for exercise and sexual activity.
Moving Forward: Being "cleared" does not mean you are ready to run a marathon. It means your wounds are closed. Re-entry into fitness should be slow and intentional. Use our Postpartum Recovery Checklist to ensure you have addressed all aspects of your healing before jumping back into a busy routine.
Frequently Asked Questions (FAQ)
Q: My bleeding stopped but started again in Week 4. Is that normal? A: It can be. sometimes the "scab" where the placenta was attached comes off, causing a brief return of bright red blood. However, if you soak a pad in an hour or pass large clots, call your doctor immediately. It could also be your period returning if you are not exclusively breastfeeding.
Q: When will my belly go down? A: Your uterus shrinks significantly by week 6, but the abdominal skin and muscles take longer to recover. It is normal to look a few months pregnant for a while.
Q: I still feel pain during sex after 6 weeks. What should I do? A: This is very common due to hormonal dryness or scar tissue. Use plenty of lubrication. If pain persists, ask your doctor about pelvic floor physical therapy.
A Note on Patience
Your journey is unique. Some days you will feel like a superhero; other days, you might stay in pajamas until noon. Both are valid. Treat yourself with the same tenderness you give your newborn. You are healing, growing, and learning all at once.
References and Further Reading
- ACOG Postpartum Care: American College of Obstetricians and Gynecologists
- Mayo Clinic - Postpartum Health: Mayo Clinic Guide
Medical Disclaimer
This article is for informational and educational purposes only and is based on general medical guidelines. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or your postpartum recovery.
About the Author
Abhilasha Mishra is a health and wellness writer specializing in women's health, fertility, and pregnancy. With a passion for empowering individuals through evidence-based information, she writes to make complex health topics accessible and actionable.