Low Milk Supply — Causes & Fixes
A clear, compassionate guide for mothers worried about low milk supply. Learn what truly causes supply issues, what is normal, how to increase milk gently, and when medical support is needed.
Try Related Tools
Use our medically reviewed calculators to get accurate insights.
Table of Contents
- What “Low Milk Supply” Really Means
- Common Causes of Low Milk Supply
- Signs That May Suggest True Low Milk Supply
- What Is Normal (and Often Misread as Low Supply)
- Gentle, Evidence-Based Ways to Increase Milk Supply
- Supplements and Galactagogues: What to Know
- When Formula Supplementation May Be Needed
- Emotional Impact of Low Milk Supply
- When to Seek Professional Help
- FAQs
- 1. How do I know if my milk supply is truly low?
- 2. Can stress really reduce milk supply?
- 3. Is pumping necessary to increase supply?
- 4. Do soft breasts mean low milk?
- 5. Can I rebuild milk supply after it drops?
- 6. Does drinking more water increase milk?
- 7. Is mixed feeding harmful?
- 8. When should I stop trying to increase supply?
- References and Further Reading
- About the Author
What “Low Milk Supply” Really Means
True low milk supply occurs when the body consistently does not produce enough milk to meet a baby’s nutritional needs, resulting in poor weight gain or dehydration. Many doctors explain that this is much less common than mothers believe.
Perceived low supply often comes from:
- Frequent feeding
- Cluster feeding
- Soft breasts
- A baby who wants comfort nursing
These signs alone do not mean your supply is low.
If you are unsure, tools like the Baby Feeding Amount Calculator can help you understand typical intake ranges based on age and weight.
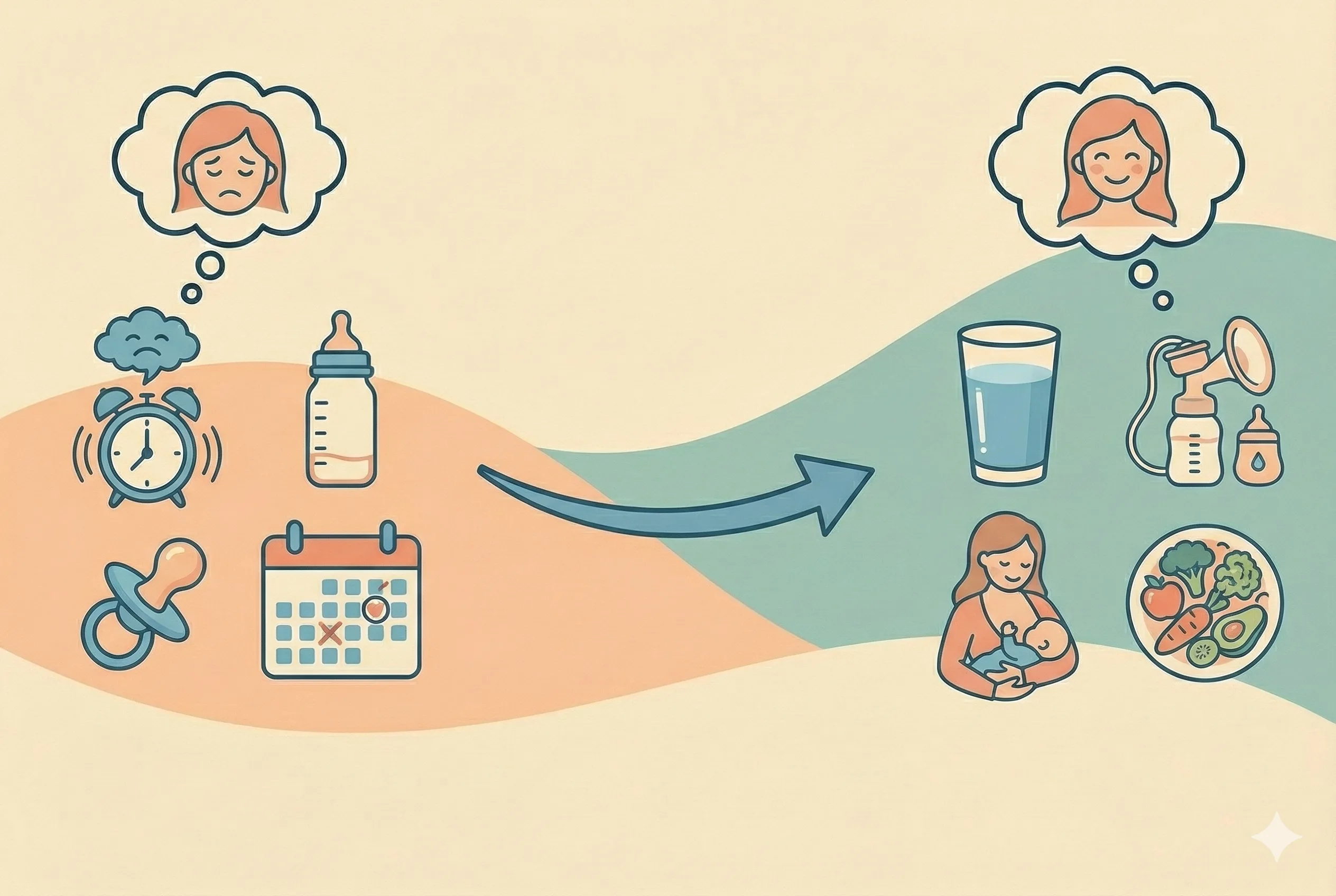
Common Causes of Low Milk Supply
1. Infrequent or ineffective milk removal
Milk production works on supply and demand. When milk is not removed often or thoroughly, the body receives a signal to slow production.
This may happen due to:
- Poor latch
- Short feeds
- Skipped night feeds
- Limited pumping sessions
2. Delayed breastfeeding initiation
Research suggests that initiating breastfeeding within the first hour after birth supports long-term milk production. Delays due to medical interventions or separation can impact early supply.
3. Hormonal and medical factors
Certain conditions can affect supply, including:
- Polycystic ovarian syndrome (PCOS)
- Thyroid disorders
- Diabetes
- Retained placental fragments
- Significant postpartum hemorrhage
These are not failures. They are medical realities that deserve support.
4. Insufficient maternal nutrition
Breastfeeding requires additional energy. Many doctors recommend adequate calories, hydration, and rest to support milk production. You can assess your intake using the Breastfeeding Calorie Needs Calculator.
5. Stress and exhaustion
Chronic stress raises cortisol levels, which can interfere with oxytocin, the hormone responsible for milk let-down. Emotional well-being matters more than many mothers are told.
6. Over-supplementation
Frequent formula supplementation without pumping can reduce demand signals, leading to a gradual drop in supply.
Signs That May Suggest True Low Milk Supply
While behavior alone is unreliable, certain signs deserve attention:
- Fewer than 6 wet diapers per day after the first week
- Poor or stagnant weight gain
- Very dark urine
- Persistent lethargy
- Minimal swallowing sounds during feeds
If you notice these, consult a pediatrician or lactation specialist promptly.
What Is Normal (and Often Misread as Low Supply)
Many mothers worry unnecessarily because of common breastfeeding realities:
- Breasts feeling softer over time
- Babies feeding frequently during growth spurts
- Cluster feeding in the evenings
- Babies wanting to nurse for comfort
Experts often explain that these are healthy patterns, not warning signs.
Gentle, Evidence-Based Ways to Increase Milk Supply
1. Feed or pump more often
Milk removal is the strongest driver of production. Aim for:
- 8–12 feeds or pumping sessions daily
- Including at least one night session
2. Improve latch and positioning
A shallow latch limits milk removal. A lactation consultant can assess and correct this quickly. Even small adjustments can make a noticeable difference.
3. Use breast compression
Gently compressing the breast during feeding helps maintain milk flow and improves transfer.
4. Prioritize maternal nourishment
Your body needs fuel. Many doctors recommend:
- Balanced meals
- Healthy fats
- Adequate protein
- Consistent hydration
If breastfeeding causes discomfort, the Breast Care & Pain Relief Guide offers practical support.
5. Rest and skin-to-skin contact
Skin-to-skin contact stimulates prolactin and oxytocin. Even brief daily sessions can support supply and emotional connection.
6. Pump strategically
If pumping, try:
- Pumping 10–15 minutes after feeds
- Power pumping sessions a few times a week
- Ensuring proper flange size
7. Address underlying medical issues
If supply does not improve, testing thyroid function or hormone levels may be appropriate.
Supplements and Galactagogues: What to Know
Herbs like fenugreek, moringa, or blessed thistle are commonly discussed. Research suggests mixed results. Some women notice improvement, others do not.
Always consult a healthcare provider before using supplements, especially if you have:
- Thyroid conditions
- Diabetes
- A history of allergies
Supplements support milk removal, they do not replace it.
When Formula Supplementation May Be Needed
Supplementation does not mean failure. Sometimes it is the safest choice for baby and mother.
If supplementation is needed:
- Continue breastfeeding or pumping to protect supply
- Use paced bottle feeding
- Work with a professional to create a plan
For mothers transitioning feeding methods, the Formula Transition Guide provides step-by-step guidance.
Emotional Impact of Low Milk Supply
Many mothers carry guilt, grief, or shame when breastfeeding does not go as planned. These feelings are real and valid.
Milk supply does not define your worth or your bond with your child. Feeding is about nourishment, connection, and safety. Babies thrive on responsive care, not perfection.
Tools like the Breastfeeding Journey can help you track progress and feel more grounded during this phase.
When to Seek Professional Help
Reach out to a lactation consultant or doctor if:
- Baby is not gaining weight
- Supply does not improve after consistent effort
- Feeding is painful
- You feel overwhelmed or distressed
Early support often prevents long-term stress.
FAQs
1. How do I know if my milk supply is truly low?
Look at weight gain and diaper output, not feeding frequency alone.
2. Can stress really reduce milk supply?
Yes. Chronic stress can interfere with let-down and overall production.
3. Is pumping necessary to increase supply?
It can help, especially if feeds are missed or supplementation is used.
4. Do soft breasts mean low milk?
No. Soft breasts often mean your supply has regulated.
5. Can I rebuild milk supply after it drops?
In many cases, yes. Frequent milk removal and support are key.
6. Does drinking more water increase milk?
Hydration supports health, but excess fluids do not directly boost supply.
7. Is mixed feeding harmful?
Not inherently. With guidance, many babies thrive with combined feeding.
8. When should I stop trying to increase supply?
If efforts cause distress or exhaustion, discuss sustainable options with your provider.
References and Further Reading
-
American Academy of Pediatrics:
https://www.healthychildren.org -
La Leche League International:
https://www.llli.org -
World Health Organization — Breastfeeding:
https://www.who.int/health-topics/breastfeeding
Medical Disclaimer
This article is for informational purposes only and does not replace professional medical advice. Always consult your healthcare provider regarding feeding concerns or medical conditions.
About the Author
Abhilasha Mishra writes about toddler learning, early development, and gentle parenting. Her goal is to support mothers with warm, practical guidance backed by trusted research.