The Gestational Diabetes Meal Plan: A Medical Guide to What to Eat and Avoid
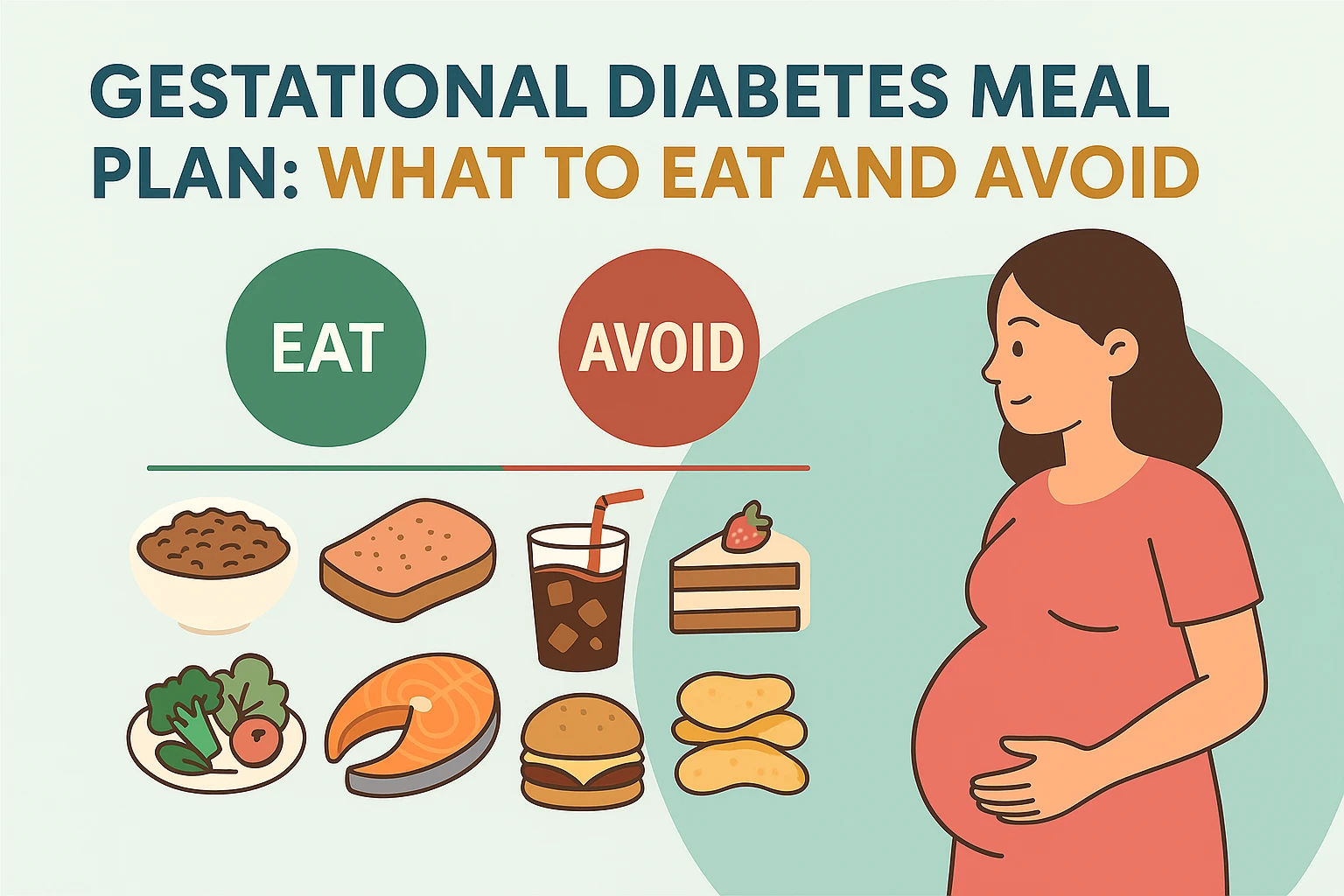
A GDM diagnosis is scary, but manageable. This E-A-T guide explains *what* to eat and *what* to avoid, focusing on carb counting, protein pairing, and a sample meal plan to manage your blood sugar.
Try Related Tools
Use our medically reviewed calculators to get accurate insights.
A diagnosis of Gestational Diabetes Mellitus (GDM) can feel overwhelming and frightening. You are immediately told your pregnancy is now "high-risk," and you may be flooded with feelings of guilt or confusion about what you did wrong.
Let's start with the most important fact, backed by all medical authorities: You did not cause this.
Gestational diabetes is not a personal failure or the result of eating too much sugar before pregnancy. It is a common medical complication caused by the powerful hormones of the placenta, which interfere with your body's ability to regulate blood sugar (insulin).
With proper management, the vast majority of women with GDM go on to have a perfectly healthy pregnancy and a healthy baby. The key is understanding what is happening in your body and how to manage it through diet, exercise, and monitoring.
This guide will explain the causes, symptoms (and lack thereof), and the essential diet plan that will become your primary tool for managing this condition.
Table of Contents
- Part 1: The "Why" — The Goal of a GDM Diet (YMYL)
- Part 2: The Most Important Tool You Must Have
- Part 3: The "Eat This" List (Your New Foundation)
- Part 4: The "Avoid This" List (The Spike Triggers)
- Part 5: The Golden Rules: A Sample GDM Meal Plan
- Part 6: Smart Snacking & Lifestyle Tips
- Part 7: Are You at Risk?
- Frequently Asked Questions (FAQ)
Part 1: The "Why" — The Goal of a GDM Diet (YMYL)
The core issue in GDM is insulin resistance.
- Hormonal Interference: To support the baby, your placenta produces hormones that, while great for the baby, make your body's cells resistant to insulin.
- Insulin's Job: Insulin is the "key" that your pancreas produces to unlock your cells, allowing glucose (sugar) from your food to enter and be used for energy.
- The Problem: In GDM, the "key" doesn't work well. Glucose gets locked out of the cells and builds up in your bloodstream, leading to high blood sugar.
- The Risk: This excess sugar crosses the placenta, causing the baby to grow too large (macrosomia) and putting them at risk for low blood sugar (hypoglycemia) after birth.
The Goal of Your New Diet: To prevent these blood sugar "spikes." You are not eliminating carbs; you are controlling them.
Part 2: The Most Important Tool You Must Have
You cannot manage what you don't measure. The only way to know how your body reacts to a specific food is to test your blood sugar.
Your doctor will prescribe a glucometer and show you how to use it. You will typically test 4 times a day:
- Fasting: As soon as you wake up.
- 1-2 hours after breakfast.
- 1-2 hours after lunch.
- 1-2 hours after dinner.
This data is your personal instruction manual. If you eat oatmeal and your number is high, your body can't handle it. If you eat eggs and your number is low, that's a "safe" food.
- Affiliate Idea: Most insurance plans cover a glucometer, but having a second one or stocking up on affordable test strips is a smart move.
- Product Pick: Home Glucometer Kits & Test Strips
Part 3: The "Eat This" List (Your New Foundation)
Your new best friends are Protein, Fiber, and Healthy Fats. These nutrients do not spike blood sugar and, when eaten with carbs, they slow down digestion, preventing a sugar rush.
1. Lean Proteins (Eat at Every Meal)
- What: Chicken breast, turkey, fish (salmon, cod), eggs, tofu, legumes (beans, lentils).
- Why: Protein is the anchor. It has almost no impact on blood sugar and promotes satiety (feeling full), which prevents carb cravings.
2. Healthy Fats
- What: Avocado, nuts (almonds, walnuts), seeds (chia, flax), olive oil.
- Why: Fat is essential for your baby's brain development and is another powerful tool for slowing carbohydrate absorption.
3. Non-Starchy Vegetables (The "Free" Foods)
- What: Eat as much as you want of these. Leafy greens (spinach, kale), broccoli, cauliflower, cucumbers, bell peppers, green beans, zucchini, mushrooms.
- Why: They are packed with fiber and nutrients but have almost zero impact on your blood sugar. Fill half your plate with these at every meal.
4. Complex Carbs (The "Controlled" Foods)
- What: These are your healthy, high-fiber carbs.
- Examples: Quinoa, brown rice, whole-grain bread (100% whole wheat), oats (steel-cut), sweet potatoes, berries (raspberries, blueberries), beans and lentils.
- Why: The fiber forces your body to digest them slowly, leading to a gentle, low rise in blood sugar instead of a spike.
Part 4: The "Avoid This" List (The Spike Triggers)
1. Sugary Drinks (The #1 Enemy)
- What: Soda, fruit juice (even "100% juice"), sweet tea, sports drinks, sweetened coffee.
- Why: They are a liquid sugar bomb that hits your bloodstream instantly, causing a massive spike that your body cannot handle.
2. White & Refined Carbohydrates
- What: White bread, white rice, white pasta, pastries, donuts, cookies, most breakfast cereals, and crackers.
- Why: Your body treats these the same way it treats pure sugar. They have no fiber to slow them down.
3. Most Fruits (In Isolation)
- What: Grapes, bananas, mangoes, and pineapple are particularly high in sugar.
- Why: While it's "natural" sugar, your body doesn't know the difference. Fruit must be treated as a carbohydrate and paired with a protein (like an apple with peanut butter).
4. Hidden Sugars
- What: Flavored yogurts, granola bars, ketchup, BBQ sauce, and many "low-fat" salad dressings (they replace fat with sugar).
- Why: You must become a label-reader. Look for "Added Sugars" on the nutrition panel.
Part 5: The Golden Rules: A Sample GDM Meal Plan
Your doctor or dietitian will give you a specific "carb count" to aim for (e.g., 30g for meals, 15g for snacks). This plan is built on that philosophy.
The #1 Rule: NEVER Eat a "Naked" Carb. Always pair your carbohydrate with a protein or a healthy fat. This is the secret to managing GDM.
- Wrong: A slice of toast.
- Right: A slice of toast with an egg and avocado.
Sample Daily Meal Plan
- Breakfast (The Hardest Meal): Insulin resistance is highest in the morning. This meal should be low-carb and protein-heavy.
- What to Eat: Scrambled eggs with spinach and a slice of whole-grain toast with avocado.
- What to Avoid: Cereal, oatmeal, or a fruit-only smoothie (these will almost always cause a spike).
- Morning Snack (2-3 hours later):
- What to Eat: A handful of almonds and a small low-sugar fruit (like a handful of berries).
- Lunch:
- What to Eat: A large salad with grilled chicken, lots of non-starchy veggies, and a small scoop of quinoa or chickpeas. Use an olive oil & vinegar dressing.
- Afternoon Snack:
- What to Eat: A cheese stick and 100% whole-wheat crackers, OR plain Greek yogurt with a few berries.
- Dinner:
- What to Eat: A "plate-method" meal: 1/2 plate non-starchy veggies (roasted broccoli), 1/4 plate lean protein (baked salmon), 1/4 plate complex carb (a small sweet potato).
- Bedtime Snack (CRITICAL):
- What to Eat: This is essential for controlling your "fasting" number. You need a snack with protein and a small carb to keep your blood sugar stable overnight. A perfect option is a piece of cheese and a few whole-grain crackers.
Part 6: Smart Snacking & Lifestyle Tips
1. Find Safe, Sugar-Free Snacks
This is where GDM is hardest. You crave carbs, but need safe options.
- Affiliate Idea: Sugar-Free & Keto-Friendly Snacks are your secret weapon. They are designed to be high in protein and fat with almost zero carbs, making them perfect GDM-friendly snacks.
- Other Ideas: Nuts, seeds, cheese, beef jerky, hard-boiled eggs, and veggies with hummus.
2. Walk After You Eat
This is a "magic" trick for lowering blood sugar. After your main meals, go for a gentle 10-15 minute walk. This activates your muscles, which pull sugar from your bloodstream for energy, dramatically reducing the post-meal spike.
Part 7: Are You at Risk?
If you are early in your pregnancy and haven't been screened yet, it's helpful to know your personal risk factors.
Check Your Personal Risk
Your age, weight, and family history all play a role. Use our Gestational Diabetes Risk Checker to understand your personal risk profile and discuss it with your doctor.
Frequently Asked Questions (FAQ)
Q: Did I cause my GDM by eating too much sugar? A: No. While a pre-existing diet high in sugar can lead to insulin resistance, GDM itself is caused by the placenta's hormones interfering with your body's insulin. Thin, healthy women get GDM, and overweight women sometimes do not. It is a complex mix of genetics, hormones, and baseline health.
Q: Will gestational diabetes go away after I give birth? A: Yes, for the vast majority of women. Once the placenta is delivered, the source of the insulin-blocking hormones is gone. Your blood sugar levels typically return to normal very quickly. Your doctor will re-test you around 6 weeks postpartum to confirm.
Q: If I have GDM, what are the risks to my baby? A: If GDM is uncontrolled, the main risk is that the excess sugar in your blood crosses the placenta, causing the baby to grow too large (macrosomia). This increases the risk of a difficult vaginal delivery, C-section, and shoulder dystocia. It also causes the baby's pancreas to overproduce insulin, which can lead to dangerously low blood sugar (hypoglycemia) for the baby right after birth.
- This is why management is key: By controlling your blood sugar, you prevent these complications.
Q: What is the risk to me after pregnancy? A: Having GDM means you have a "failed" your body's stress test. It reveals an underlying predisposition. Women who have had GDM have a significantly higher risk (up to 50%) of developing Type 2 diabetes later in life. This makes long-term healthy eating and exercise a lifelong priority.
Medical Disclaimer
This article is a medical guide intended for informational and educational purposes only. It is not a substitute for professional medical advice from your obstetrician or endocrinologist. Your GDM management plan, including diet and blood sugar targets, must be personalized by your healthcare team.
About the Author
Abhilasha Mishra is a health and wellness writer specializing in women's health, fertility, and pregnancy. With a passion for empowering individuals through evidence-based information, she writes to make complex health topics accessible and actionable.