Calories Needed While Breastfeeding
A warm, evidence-based guide to understanding calorie needs while breastfeeding. Learn how much energy your body truly requires, how needs change over time, signs you may be under-fueling, and how to nourish yourself without guilt or fear.
Try Related Tools
Use our medically reviewed calculators to get accurate insights.
Table of Contents
- Why Breastfeeding Requires Extra Calories
- Average Calorie Needs While Breastfeeding
- How Calorie Needs Change Over Time
- Signs You May Not Be Eating Enough
- Does Eating More Increase Milk Supply?
- What Kind of Calories Matter Most
- Breastfeeding, Weight Loss, and Realistic Expectations
- Emotional Hunger and Breastfeeding
- When Combination Feeding Changes Calorie Needs
- When to Seek Professional Advice
- FAQs
- 1. How many extra calories do I really need while breastfeeding?
- 2. Can eating too little reduce milk supply?
- 3. Should I count calories while breastfeeding?
- 4. Is it safe to diet while breastfeeding?
- 5. Do breastfeeding cravings mean I lack nutrients?
- 6. Will my appetite decrease when breastfeeding less?
- 7. Does breastfeeding burn fat automatically?
- 8. When should calorie intake return to pre-pregnancy levels?
- References and Further Reading
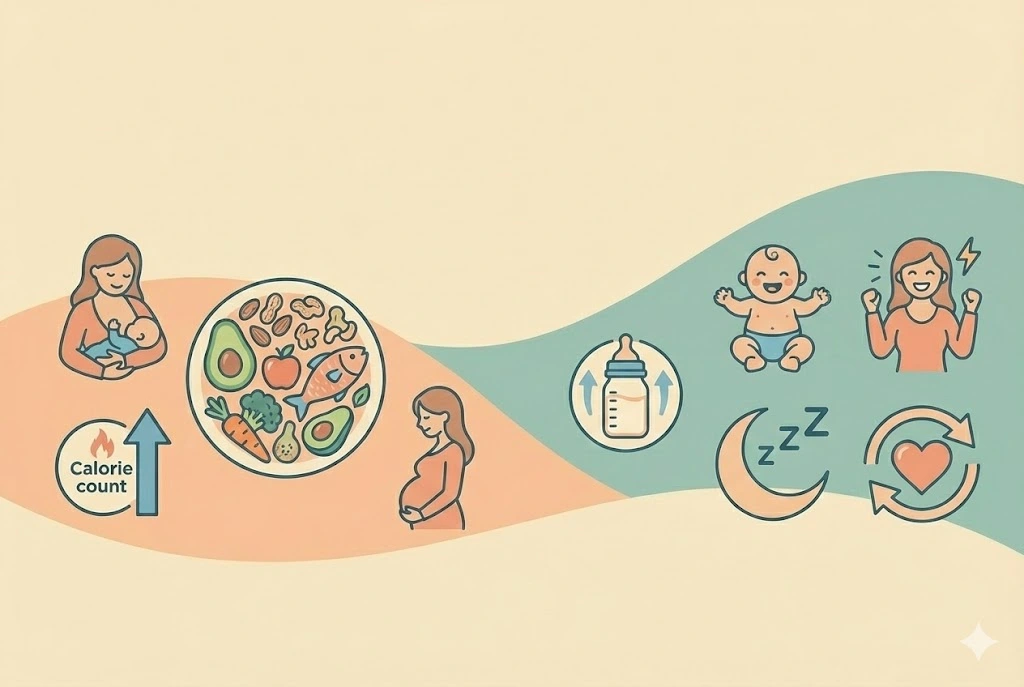
Why Breastfeeding Requires Extra Calories
Producing breast milk is not passive. Your body is actively converting nutrients into milk around the clock. Research suggests that exclusive breastfeeding uses approximately 450 to 500 extra calories per day during the first six months.
These calories are not just burned. They are invested in:
- Milk production
- Hormonal balance
- Tissue repair after birth
- Emotional regulation and energy levels
Many doctors recommend thinking of breastfeeding as comparable to a moderate daily workout that never truly ends.
Average Calorie Needs While Breastfeeding
Calorie needs depend on your body size, activity level, feeding frequency, and whether breastfeeding is exclusive or combined.
General guideline ranges
- Non-breastfeeding adult woman: ~1,800–2,000 calories
- Breastfeeding mother (exclusive): ~2,300–2,700 calories
- Breastfeeding with higher activity or twins: often higher
These are averages, not rules. Some women require more, others slightly less. Listening to your body remains essential.
For personalized estimates, the Breastfeeding Calorie Needs Calculator can help translate general guidance into your daily reality.
How Calorie Needs Change Over Time
First 0–3 months postpartum
This is when calorie demand is often highest. Milk supply is being established, healing is ongoing, and sleep deprivation adds stress.
3–6 months
Milk production stabilizes, but calorie needs remain elevated, especially during growth spurts.
6 months and beyond
As solids are introduced, milk intake may slowly decline, but many mothers still require additional calories if breastfeeding continues frequently.
Experts often explain that hunger spikes are common and usually meaningful signals rather than habits to suppress.
Signs You May Not Be Eating Enough
Undereating while breastfeeding is more common than many realize, especially when mothers are trying to lose pregnancy weight.
Possible signs include:
- Constant fatigue despite rest
- Feeling shaky, dizzy, or irritable
- Sudden drops in milk supply
- Intense sugar cravings
- Difficulty concentrating
- Frequent headaches
If milk output feels unpredictable, reviewing feeding volume with the Baby Feeding Amount Calculator may provide helpful context.
Does Eating More Increase Milk Supply?
Eating enough supports milk production, but eating excessively does not automatically increase supply. Milk supply responds primarily to demand, meaning how often and effectively milk is removed.
However, consistently under-fueling your body can contribute to:
- Slower letdown
- Lower energy for feeding sessions
- Hormonal disruption
Many doctors recommend focusing on adequacy rather than excess.
What Kind of Calories Matter Most
Calories are not all equal in how they support breastfeeding.
Nutrients that matter most
- Protein for tissue repair and milk synthesis
- Healthy fats for milk quality
- Complex carbohydrates for sustained energy
- Iron and calcium for maternal health
Whole foods are helpful, but perfection is not required. Nourishment, not restriction, is the goal.
If you experience breast discomfort or engorgement while adjusting feeding or pumping routines, the Breast Care & Pain Relief Guide offers gentle strategies.
Breastfeeding, Weight Loss, and Realistic Expectations
Some women lose weight while breastfeeding. Others maintain or even gain weight. Both patterns can be normal.
Research suggests that aggressive calorie restriction may:
- Affect mood
- Reduce milk supply
- Increase exhaustion
Weight changes often stabilize naturally after breastfeeding tapers. Trusting this phase helps protect both physical and emotional health.
Emotional Hunger and Breastfeeding
Not all hunger is purely physical. Breastfeeding alters hormones connected to comfort, bonding, and stress response. Wanting warmth, carbs, or familiar foods can be part of emotional regulation during this period.
This does not mean something is wrong. It means your nervous system is adapting.
For ongoing support and perspective, many mothers find reassurance in the Breastfeeding Journey resource.
When Combination Feeding Changes Calorie Needs
If breastfeeding is combined with formula or transitioning away from nursing, calorie needs may shift gradually.
The Formula Transition Guide can help you navigate this stage without sudden dietary changes that leave you depleted.
For broader feeding education, the Breastfeeding Guide offers stage-based insights.
When to Seek Professional Advice
Reach out to a healthcare provider or lactation consultant if:
- Milk supply drops suddenly
- You feel persistently weak or lightheaded
- Weight changes are extreme or rapid
- Feeding feels physically or emotionally overwhelming
Early support protects long-term wellbeing.
FAQs
1. How many extra calories do I really need while breastfeeding?
Most breastfeeding mothers need about 450–500 additional calories daily, though individual needs vary.
2. Can eating too little reduce milk supply?
Yes. Chronic under-eating can affect energy, hormones, and milk output.
3. Should I count calories while breastfeeding?
Many doctors recommend focusing on hunger cues rather than strict counting.
4. Is it safe to diet while breastfeeding?
Gentle, gradual changes may be appropriate, but aggressive dieting is not recommended.
5. Do breastfeeding cravings mean I lack nutrients?
Not always. Cravings can reflect energy needs, stress, or hormonal shifts.
6. Will my appetite decrease when breastfeeding less?
Often yes, but the transition is gradual.
7. Does breastfeeding burn fat automatically?
Breastfeeding increases energy use, but weight response varies by individual.
8. When should calorie intake return to pre-pregnancy levels?
Usually after breastfeeding frequency drops significantly or ends.
References and Further Reading
-
World Health Organization — Maternal Nutrition:
https://www.who.int/health-topics/breastfeeding -
American Academy of Pediatrics — Breastfeeding:
https://www.healthychildren.org -
CDC Breastfeeding Nutrition:
https://www.cdc.gov/breastfeeding
Medical Disclaimer
This article is for educational purposes only and does not replace personalized medical advice. Always consult your healthcare provider regarding nutrition, milk supply, or postpartum health concerns.
About the Author
Abhilasha Mishra writes about early childhood development, women’s health, and parenting. Her work focuses on empathy, clarity, and practical guidance for mothers navigating the toddler years.