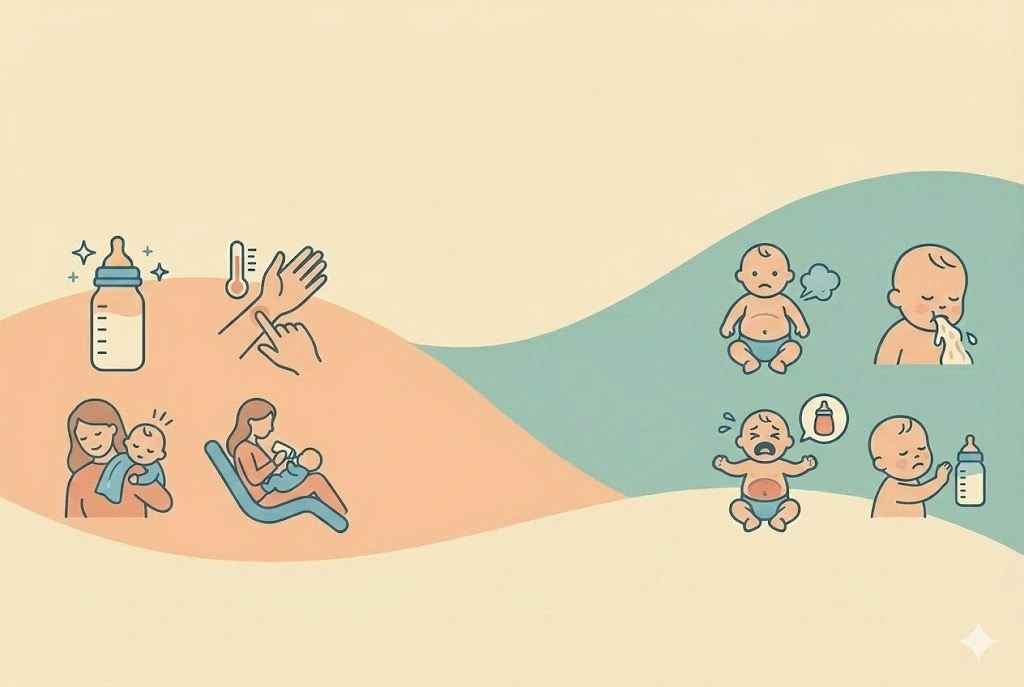
Bottle Feeding Guide And Overfeeding Signs
A clear, medically responsible guide for mothers using bottles, whether with formula or expressed breast milk. Learn how to bottle-feed safely, recognize hunger and fullness cues, avoid overfeeding, and build a calm, confident feeding routine.
Try Related Tools
Use our medically reviewed calculators to get accurate insights.
Table of Contents
- What Bottle Feeding Really Means
- Hunger and Fullness Cues in Bottle-Fed Babies
- How Much Should a Bottle-Fed Baby Eat?
- The Importance of Paced Bottle Feeding
- Common Overfeeding Signs to Watch For
- Why Overfeeding Happens More Easily With Bottles
- How to Prevent Overfeeding Gently
- Bottle Feeding and Combination Feeding
- Switching Between Breast and Bottle
- When to Seek Medical Advice
- Emotional Side of Bottle Feeding
- FAQs
- 1. Can bottle-fed babies overeat?
- 2. Should I always finish the bottle?
- 3. Is spit-up always a sign of overfeeding?
- 4. How do I know if the nipple flow is too fast?
- 5. Can paced feeding help reflux?
- 6. Is combination feeding safe?
- 7. Does bottle feeding affect future eating habits?
- 8. When should I change bottle size?
- References and Further Reading
What Bottle Feeding Really Means
Bottle feeding can include:
- Exclusive formula feeding
- Expressed breast milk
- Combination feeding
Regardless of what is in the bottle, the principles remain the same. Babies are born with natural hunger and fullness cues. Bottle feeding works best when it respects those cues instead of encouraging finishing a set amount.
If you want help understanding age-appropriate intake ranges, the Baby Feeding Amount Calculator can be a useful reference.
Hunger and Fullness Cues in Bottle-Fed Babies
Early hunger cues
- Lip smacking
- Turning head side to side
- Sucking on hands
- Becoming alert and restless
Fullness cues
- Slowing sucking
- Relaxed hands
- Turning head away
- Pushing the bottle out with the tongue
- Falling asleep calmly
Experts often explain that stopping a feed when fullness cues appear helps protect digestion and supports long-term appetite regulation.
How Much Should a Bottle-Fed Baby Eat?
While exact needs vary, these ranges are commonly used by pediatricians:
Newborn to 1 month
- 1.5–3 oz per feed
- 8–12 feeds per day
1–3 months
- 3–4 oz per feed
- 7–9 feeds per day
3–6 months
- 4–6 oz per feed
- 5–7 feeds per day
These are averages, not rules. Growth spurts, illness, and sleep changes can temporarily alter intake.
For mothers who are pumping, calorie needs can change as feeding patterns shift. The Breastfeeding Calorie Needs Calculator can help you adjust nutrition during this phase.
The Importance of Paced Bottle Feeding
Paced bottle feeding helps mimic breastfeeding flow and gives babies time to recognize fullness.
How to practice paced feeding
- Hold your baby upright
- Keep the bottle horizontal
- Allow pauses every few minutes
- Watch cues instead of the bottle level
This approach reduces gas, reflux, and overfeeding risk.
Common Overfeeding Signs to Watch For
Overfeeding does not always mean feeding too much in one sitting. It can also mean feeding too often without allowing digestion.
Physical signs
- Frequent spit-up or vomiting
- Gassiness and bloating
- Fussiness shortly after feeds
- Arching the back during or after feeding
Digestive signs
- Watery stools
- Discomfort after every feed
- Excessive hiccups
Behavioral signs
- Wanting to suck constantly without hunger cues
- Crying that worsens after feeding
Many doctors recommend checking feeding pace before reducing volume.
Why Overfeeding Happens More Easily With Bottles
Bottles flow faster than breasts. Milk continues to flow even when babies slow down.
Common reasons include:
- Encouraging bottle finishing
- Fast-flow nipples
- Feeding as the first response to all fussing
- Feeding to soothe without checking cues
These habits are understandable, especially for tired parents.
How to Prevent Overfeeding Gently
1. Respect pauses
If your baby pauses, wait. Do not rush the next sip.
2. Check nipple flow
A nipple that drips when inverted may be too fast for your baby’s age.
3. Use feeding for hunger, not every cry
Babies cry for many reasons. Comfort, diaper changes, or closeness may be what they need.
4. Avoid pressure
You do not need to finish every bottle. Babies know when they are done.
Bottle Feeding and Combination Feeding
Many families combine bottle and breast feeding. This works well with mindful pacing.
If breastfeeding causes soreness or engorgement during pumping phases, the Breast Care & Pain Relief Guide offers relief strategies.
For guidance on maintaining supply while bottle feeding, explore the Breastfeeding Guide and Breastfeeding Journey tools.
Switching Between Breast and Bottle
Transitions can feel emotional. Some babies adapt easily, others need time.
Helpful tips:
- Use slow-flow nipples
- Keep bottle feeding calm and upright
- Let another caregiver offer bottles initially
- Avoid forcing feeds
If you are transitioning fully, the Formula Transition Guide provides step-by-step support.
When to Seek Medical Advice
Consult your pediatrician if:
- Spit-up becomes forceful or projectile
- Weight gain is excessive or poor
- Feeding always causes distress
- Baby appears uncomfortable most of the day
Early guidance prevents unnecessary discomfort.
Emotional Side of Bottle Feeding
Some mothers worry bottle feeding may affect bonding. Research suggests bonding depends on responsiveness, touch, and presence, not the feeding method.
Holding your baby close, making eye contact, and feeding calmly builds secure attachment.
FAQs
1. Can bottle-fed babies overeat?
Yes, especially if feeds are rushed or cues are ignored.
2. Should I always finish the bottle?
No. Stop when your baby shows fullness cues.
3. Is spit-up always a sign of overfeeding?
Not always. Mild spit-up can be normal. Persistent discomfort deserves evaluation.
4. How do I know if the nipple flow is too fast?
If milk drips freely or your baby coughs or gulps, the flow may be too fast.
5. Can paced feeding help reflux?
Many doctors recommend paced feeding to reduce reflux symptoms.
6. Is combination feeding safe?
Yes. With proper pacing and supply support, many babies thrive.
7. Does bottle feeding affect future eating habits?
Responsive feeding supports healthy appetite regulation later in life.
8. When should I change bottle size?
Change based on feeding duration and cues, not age alone.
References and Further Reading
-
American Academy of Pediatrics:
https://www.healthychildren.org -
World Health Organization — Infant Feeding:
https://www.who.int/health-topics/infant-nutrition -
CDC Infant Nutrition:
https://www.cdc.gov/nutrition/infantandtoddlernutrition
Medical Disclaimer
This article is for educational purposes only and does not replace professional medical advice. Always consult your healthcare provider regarding feeding concerns or symptoms.
About the Author
Abhilasha Mishra writes about early childhood development, women’s health, and parenting. Her work focuses on empathy, clarity, and practical guidance for mothers navigating the toddler years.